Total Knee Joint Replacement
Knee Anatomy & Function
A Normal Knee
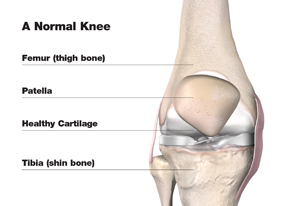
- The lower end of the thigh bone, or femur.
- The upper end of the shin bone, or tibia.
- The kneecap, or patella.
The thigh bone (femur) turns on the upper end of the shin bone (tibia), and the kneecap (patella) slides in a groove on the end of the thigh bone. Ligaments, which are bands of tissue, connect the thigh bone and the shin bone to help keep the knee joint steady. The quadriceps, the long muscles on the front of the thigh, help strengthen the knee.
A smooth substance called articular cartilage covers the surface of the bones where they touch each other within the joint. This articular cartilage acts as a cushion between the bones. The rest of the surfaces of the knee joint are covered by a thin, smooth tissue liner called synovial membrane, which makes a small amount of fluid that acts as a lubricant so that the joint bones will not rub against each other.
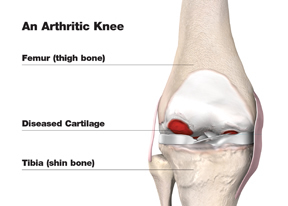
An Arthritic Knee
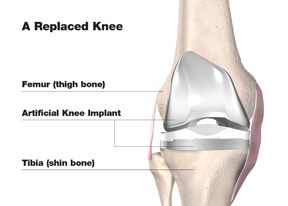
A Replaced Knee
Knee replacement surgery may provide the pain relief you long for and enable you to return to the things you enjoy doing. Remember, even if your doctor recommends knee replacement for you, it is still up to you to make the final decision. The ultimate goal is for you to be as comfortable as possible with your choice — and that always means making the best decision based on your own individual needs.
If you do choose surgery, you’ll be in good company: More than a quarter-million Americans have knee replacement surgery every year.1 First performed in 1968, the procedure typically relieves pain and restores joint function.
- 1. Arthritis Foundation – February 2006
Knee Surgery Candidates
Knee surgery may be suitable for patients who:
- Have a painful, disabling joint disease of the knee resulting from a severe form of arthritis
- Are not likely to achieve satisfactory results from less invasive procedures, medication, physical therapy, or joint fluid supplements
- Have bone stock that is of poor quality or inadequate for other reconstructive techniques.
Knee Surgery Procedure
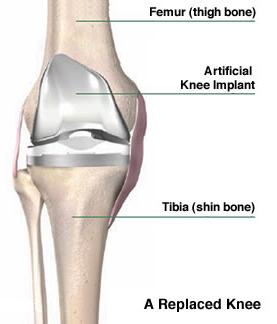
The tibia (shin bone) is prepared with a flat cut on the top. The exposed end of the bone is sized to fit the metal and plastic tibial components. The metal tibial component is inserted into the bone. Then a plastic insert is snapped into the tibial component. The femoral component will slide on this plastic as you bend your knee.
If needed, the patella (kneecap) is also cut flat, and fitted with a plastic patellar component. Bone cement may be used to help secure the implants onto your bone. Your surgeon will conduct several tests during the surgery to ensure the correct sized components are used to help you regain good balance and motion in your knee. Your surgeon will then close the wound in layers with stitches and/or staples.
Recovery
Every individual is different and every treatment plan is different. The length of hospital stay after joint replacement varies and depends on many factors including age and physical ability.
Estimated Recovery Schedule:
- In-hospital Recovery: 2 – 5 days
- Significant Functional Improvement: 6 weeks – 3 months
- Maximal Improvement: 6 – 12 months
Rehabilitation
Following joint replacement the physical therapist begins an exercise program to be performed in bed and in the therapy department. The physical therapist or another member of the staff works with the patient to help the patient:
- Regain muscle strength
- Increase range of motion
Animations
FAQ
Frequently asked questions about Knee Replacement
This is a very personal decision that only you can make with the help of an orthopaedic specialist’s evaluation of your pain and its effects on your daily life. For example, experiencing knee pain day after day without relief can lead to “staying off” the joint — which often weakens the muscles around it, so it becomes even more difficult to move.
When other more conservative treatment options — including medication and physical therapy — no longer provide pain relief, joint replacement may be recommended.
The MIS knee replacement technique is significantly less invasive than conventional knee replacement surgery, but it is still a major surgery.
As with any major surgical procedure, patients who undergo total joint replacement are at risk for certain complications, the vast majority of which can be successfully avoided and/or treated.
Following joint replacement surgery, hospital stays vary depending on insurance coverage and individual medical status. A total of four days (including the day of the surgery) is typical. On the first day after your surgery, you will likely get out of bed and begin physical and occupational therapy, typically several brief sessions a day.
Usually a case manager is assigned to work with you as you move through your rehabilitation routines. When you’re ready for discharge, the decision will be made concerning whether you can best continue to recover at home (the usual procedure) or in another facility where you may receive specialized rehabilitative help. If you do go to another facility, the goal will be to return you to your home, able to move about with a safe level of independence, within three to five days.
In surgery, the knee is flexed and the leg suspended. One muscle is separated to expose the femur (thighbone); later, the tibia (shinbone) is exposed. The damaged surfaces at the end of the thighbone are trimmed to shape it to fit inside the total knee prosthesis. The shinbone is cut flat across the top and a hole is created in the center to hold the stem of the tibial component. If needed, the knee cap is trimmed and the patellar component attached.
At various points during surgery, the alignment, function, and stability of the knee joint are evaluated and required adjustments are made. The prosthesis components are cemented into place, any contracted ligaments are released, the midvastus muscle is reconstructed, and the incision is closed.
Learn More
The following information is provided by the American Academy of Orthopaedic Surgeons.

